Osteoarthritis: Debunking Common Myths
If you have been diagnosed as having osteoarthritis (OA) then you are not alone. In fact, OA is one of the leading causes of disability affecting almost 250 million people worldwide. There are many common misconceptions about OA and the people who suffer from its effects. This article will debunk 5 of the most common myths about OA
Myth 1: OA is wear and tear due to aging
OA used to be thought of as a degenerative disease of wear and tear because of aging. It is now recognized that OA is a disorder involving multiple systems both inflammatory and biomechanical in nature. It is not just age which causes OA. Some of the other risk factors which affect OA are sex (it is more common in females), genetic factors, obesity, and diabetes to mention a few. OA can occur after a traumatic event but it can also be idiopathic
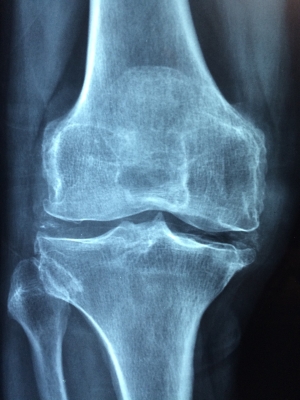
Myth 2: The source of pain in OA is degeneration of the cartilage of the joint
Although we used to think about the cartilage as the source of pain in OA, we now know the source of pain can also be derived from changes to the non-cartilaginous components of the joint. The joint capsule, synovium, subchondral bone, ligaments, and periarticular muscles (see picture below) may also be involved in producing pain in OA.
Myth 3: The more OA changes one sees on X-ray, the more pain a patient will feel
X-ray is the best investigation to review OA changes. Saying that, structural changes seen on scans are not enough to produce pain. Most people over 40 years of age will present with some changes on scans, just like most people over 40 have wrinkles. Degenerative changes are part of normal life and are not always painful. Some people may have significant OA changes seen on their scans, but have very little pain. Pain is much more about sensitivity of the nervous system then damage of a joint
Although structural change is not something that can be reversed, it is only one part of the pain puzzle. Pain is multidimension and complex. Many things influence a patient's pain level. Some of these include emotional stress, physical load, genetics, thoughts, emotions and mental health.
Myth 4: Exercise is bad for OA and can make it worse
Joints like stress. Load keeps them healthy. Humans can adapt to load and get stronger. Research shows that normal loading doesn't seem to aggravate OA and is safe. Inactivity and disuse are deleterious for the health of the knee joint. The absence of mechanical stimulation can induce a more rapid cartilage degeneration due to cartilage softening/ thinning, decrease of glycosaminoglycan (an important compound found in cartilage) content, impaired joint mechanics and flexibility.
Despite that, not every exercise will be good or useful for those with OA. Each person can benefit from a tailor-made strength and movement program created by a physiotherapist who has fully assessed your specific situation.
This article showed that in addition to the symptom-modifying effects of exercise, there is evidence of exercise exerting disease-modifying effects. For example, increased physical activity in the form of aerobic and weight-bearing exercises resulted in increased proteoglycan content, one of the major components of the cartilage extracellular matrix, in the cartilage of OA patients. Strength training for 30 months, compared to range of motion exercises alone, resulted in a decreased mean rate of joint space narrowing
Myth 5: If I have a painful joint, I should see an orthopedic surgeon
Most patients tend to book to see an orthopedic surgeon when they experience pain in their musculoskeletal system. Although there are many things that an orthopedic surgeon may offer for OA patients, the first port of call of most OA patients should be a physiotherapist. The reasons for this are:
- Through a variety of subjective questioning and objective testing, a physio will be able to differentially diagnose whether you have OA or another condition.
- The role of a physiotherapist is to treat patients with OA using a variety of modalities (for example massage, taping, acupuncture). These modalities help reduce pain and make it easier to strengthen the joint.
- A physiotherapist is the best person to help and advise on which exercises a patient should and should not be doing.
- If a patient is not a candidate for surgery, an orthopedic surgeon will often refer an OA patient to physiotherapy anyway as this is the most conservative option and can often help.
Links to articles mentioned above:
www.ncbi.nlm.nih.gov/pmc/articles/PMC6179584/pdf/jpr-11-2189.pdf
www.ncbi.nlm.nih.gov/pmc/articles/PMC4350574/pdf/nihms643856.pdf




Comments